Vision is one of nature’s great gifts. It’s essential to safety, work, and living a meaningful life. But vision is often compromised when traumatic brain injury (TBI) occurs, leaving patients with deficits that require specialized clinical care. Head trauma can cause serious vision impairments. It may also affect hearing, mobility, and may damage the vestibular and proprioception systems (which provide a sense of balance and spatial orientation). All these systems are interconnected with vision. Other trauma-induced visual problems may include:
Double-vision; limited field of vision
Eyes that do not track objects correctly
Uncoordinated eye and body movements
Sensitivity to light; fatigue
Poor depth perception
Difficulty reading
To identify and treat these deficits, Centre for Neuro Skills offers the clinical services of Carl Garbus, O.D., a California optometrist who works in the field of neuro-optometry. Dr. Garbus works with CNS patients from the Bakersfield and Los Angeles clinics.
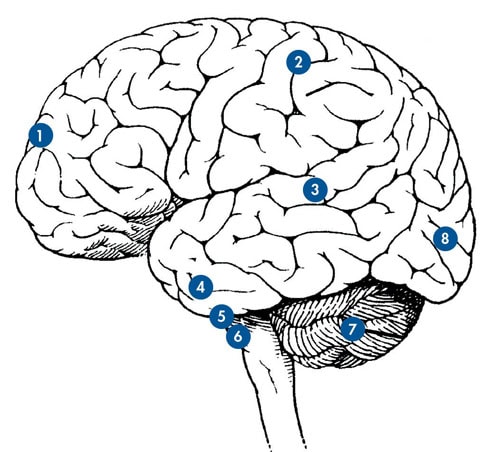
The occipital lobe, where most visual information is processed, is located at the back of the head. Eighty percent of visual input travels through many parts of the brain to arrive at this lobe. There may be damage all along that pathway. Thus, Dr. Garbus needs to know what input the brain is receiving from the eyes.
Initially two appointments are made. Each is two hours long and includes exams determining field of vision, mobility, eye movements, postural movement, and balance. He prepares for each appointment by reviewing patient records, medical history, medication, and extent of injury. CNS therapists accompany patients to their appointments, so they may better support this aspect of rehabilitation.
On the first visit, he checks eye health, the optic nerve, retina, macula, and blood vessels. On the second, he works on function, ambulation, gait, balance, and the patient ’s sense of space. To further understand TBI-related impairment, another test is administered which involves an advanced technology called the Visual Evoked Potential (VEP). This is an electro diagnostic test that measures brainwaves associated with the visual pathways. If there is damage along the pathway, the electrical signal in the occipital lobe may be adversely affected.
Creating New Pathways in the Brain
“Along with the different therapies provided at CNS, these procedures and techniques can create new pathways in the brain,” Dr. Garbus said. Progress evaluations help him and CNS clinicians measure improvement and revise therapies. “These evaluations involve more than a typical eye exam,” Dr. Garbus noted. “We have to adjust for speed of processing, dizziness, light sensitivity, and fatigue to identify and treat vision deficits.”
Understanding stroke and TBI are crucial in prescribing glasses specially designed for TBI patients. This usually involves lenses that address specific vision problems, or it may require “prism” glasses to correct visual spatial orientation and eye teaming deficits.
Vision’s Role in Returning to Work
Most patients want to work again, which is a core component of the CNS goal-oriented philosophy. In his years of working with TBI patients, these detailed strategies are worth the effort, Dr. Garbus noted. Many CNS patients return to functionality in real-world settings. “CNS is so good about working at a patient ’s own level of capacity, getting them retrained, inspiring them to volunteer, and helping them to gain a sense of self-worth,” he said.
CNS Monthly Newsletter
The latest CNS updates, including events, company information, and patient care developments
The Inside View
Quarterly magazine focused on brain injury research, rehabilitation, and advancements shaping the field
Sign-up for one or both to stay connected with brain injury news and recover