Persons with a traumatic brain injury (TBI) or cerebral vascular accident (CVA) frequently will experience symptoms of double vision, movement of print or stationary objects such as walls and floor, eye strain, visual fatigue, headaches, and problems with balance.
When someone endures a brain trauma, vision problems are often the unwelcome companion of concussion, traumatic brain injury (TBI), or stroke.
Patients may not know they have visual deficits until seemingly unrelated issues arise. An awkward gait, imbalance, problems with activities of daily living or learning impairment can be the clinician’s clue that damage is present.
Centre for Neuro Skills believes that vision therapy is an essential aspect of comprehensive care. For over 20 years, the CNS vision program has helped patients recover from post-injury visual deficits, allowing them to work, live safely, and even drive again.
“The visual system is a silent system,” said David Harrington, MBA, OTR/L, CBIST, Director of Operations at CNS. “It takes a skilled clinician to detect problems, which may linger undetected for years.”
Visual Therapies Enhance Rehabilitation
Addressing visual deficits is crucial in a successful recovery. It enhances the clinical efficiency of other therapies, since vision is connected to movement, reasoning, hearing, and speech.
“The clinical staff must understand the visual system,” David emphasized. CNS case managers and therapists are trained in this area, and they collaborate with vision specialists to maximize treatment outcome.
Some of the red flags that therapists look for are erratic eye movements or eyes that don’t converge on an object. Once vision damage is suspected, occupational therapists administer three eye screens, which assess the optic system, the visual field, and visual perception/processing information.
The screening results are used to create an individualized treatment plan that includes vision therapy, where needed. Because the brain’s spatial, visual, perceptual, and cognitive functions are all related to sight, treatment planning encompasses many disciplines that support vision.
When testing is complete, patients sometimes require vision therapy and specialized glasses, and, David notes, “a pair of standard lenses won’t do.”
CNS refers these patients to a consulting neuro optometrist who understands TBI, tests for specific optic and brain pathway damage, and prescribes lenses for each patient’s deficits.
These specialists also help refine the patient’s treatment plan, collaborating with CNS occupational, physical, and speech therapists to form a dedicated vision and rehabilitation team.
Technologies Build Skills, Support Patient Goals
“Our objective is to remediate the visual system so patients can scan the environment for hazards, read a prescription bottle, and understand directions,” David added. “When facilities don’t address vision problems, it can really delay a patient’s progress.”
To meet that objective, CNS offers tools and technologies to assess patients and correct neuro pathways.
These tools include:
Dynavision: a testing and visual rehabilitation system that determines eye function and improves acuity
Tranaglyphs: red/green glasses to strengthen 3D vision
Vectograms: polarized lenses that help eyes track together and form depth perception
The outcome of a comprehensive vision program benefits patients in the long term. A core CNS philosophy is providing patients with the skills to achieve lifelong independence. Staff works with payers, caregivers, and families to provide updates on vision tests and patient milestones along the path of rebuilding skills.
Hope in Sight: A Patient Returns to Reading, Working, Driving
In his 20 years as a CNS executive, clinician and case manager, David has seen remarkable success stories.
He recalled one man whose vision was so impaired that his eyes could only converge on objects that were ten feet from his nose. Normal convergence distance is two inches.
His visual system conflicted with his vestibular system, which caused confusion, created nausea, and increased risk of further injury. He also couldn’t dress himself or read prescriptions. In the CNS vision program, he improved convergence from ten feet to one foot, allowing him to drive, work, and abandon the cane he depended on.
Brain trauma often causes vision deficits, a frustrating reality that complicates a patient’s ability to walk, achieve balance, and return to work post injury. Because vision affects other sensory functions, these deficits can impair judgment, focus, and spatial orientation. This impacts a critical milestone in recovery – safely navigating in real world settings.
Centre for Neuro Skills has offered a comprehensive vision program for over 20 years, providing therapies and technologies that can build new pathways in the brain and correct visual damage.
Dr. Charles Shidlofsky, OD, FCOVD, is a Plano, TX neuro-optometrist who consults with the CNS Dallas facility, offering clinical expertise to people with traumatic brain injury (TBI) and stroke. He has been in practice since 1988. “It’s like physical or occupational therapy for the eyes,” he says, referring to the extensive evaluation and therapy he offers at his clinic, Neuro-Vision Associates of North Texas. “We work to rebuild function that was compromised by trauma.”
Post trauma vision syndrome and visual midline shift syndrome are the two most common issues he sees in TBI patients.
In-depth Exams Support CNS Care
To decipher the nature and extent of damage, patients come in for three initial appointments. They are:
A neuro-optometric assessment to test visual skills, eye tracking, spatial orientation, eye teaming, and convergence. Prior to this appointment, Dr. Shidlofsky thoroughly reviews the patient’s case history.
A neuro sensory exam to determine the patient’s center of balance. He isolates vision and inner ear functions to determine their affect on balance and how well the three entities integrate.
A thorough consultation to review test results with the patient and CNS occupational therapist. He recommends guidelines and goals for postacute treatment, which identify therapies to utilize at CNS.
Thereafter, Dr. Shidlofsky sees patients monthly–always with their CNS occupational therapist–to review progress.
Texas Neuro-Optometrist Brings a Vision of Hope to Patients
“It’s like physical or occupational therapy for the eyes. We work to rebuild function that was compromised by trauma. We can’t understand the visual system until we know how it interacts with other sensory systems,” he says of the assessment process.
Active and Passive Therapies Enhance Treatment
Specialized lenses are often prescribed, which use a combination of prisms, tints, and occlusion to correct trauma-induced problems. These optometric devices complement treatment at CNS. “I call the lenses ‘passive’ therapy,” he noted. “The ‘active’ therapy is treatment provided at my clinic and at CNS. Both work on specific skills. Each work together, but are separate interventions.”
In his 13 years of working with CNS, Dr. Shidlofsky has seen many TBI and stroke patients return to driving and working, which he considers a victory to celebrate. "We identify the neuro pathways that are damaged, then provide CNS patients with the tools, technology, therapies, and eye wear that bridge the gap between rehabilitation and returning to normal living,” he said.
Vision is one of nature’s great gifts. It’s essential to safety, work, and living a meaningful life. But vision is often compromised when traumatic brain injury (TBI) occurs, leaving patients with deficits that require specialized clinical care. Head trauma can cause serious vision impairments. It may also affect hearing, mobility, and may damage the vestibular and proprioception systems (which provide a sense of balance and spatial orientation). All these systems are interconnected with vision. Other trauma-induced visual problems may include:
Double-vision; limited field of vision
Eyes that do not track objects correctly
Uncoordinated eye and body movements
Sensitivity to light; fatigue
Poor depth perception
Difficulty reading
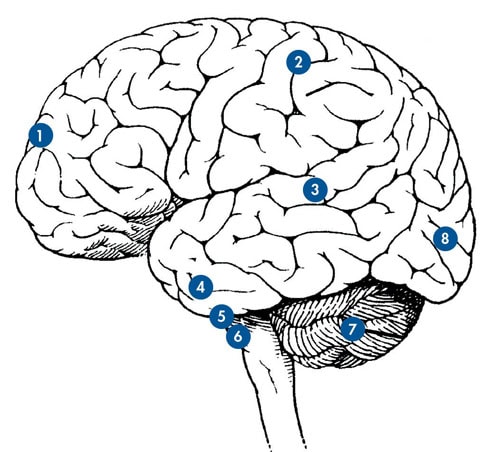
FRONTAL LOBE:
Eye Movement Planning
PARIETAL LOBE:
Visuospatial Map
Visual Attention
MIDDLE TEMPORAL LOBE:
Motion Perception
INFERIOR TEMPORAL LOBE:
Object Perception
MIDBRAIN:
Visual Orientation and Eye Movements
BRAINSTEM:
Eye Movements Integrated with Vestibular Input
CEREBELLUM:
Moderates Eye Movements
OCCIPITAL LOBE:
Shape, Contrast, Color
Exams Identify Deficits and Guide Treatment Plans
To identify and treat these deficits, Centre for Neuro Skills offers the clinical services of Carl Garbus, O.D., a California optometrist who works in the field of neuro-optometry. Dr. Garbus works with CNS patients from the Bakersfield and Los Angeles clinics.
The occipital lobe, where most visual information is processed, is located at the back of the head. Eighty percent of visual input travels through many parts of the brain to arrive at this lobe. There may be damage all along that pathway. Thus, Dr. Garbus needs to know what input the brain is receiving from the eyes.
Initially two appointments are made. Each is two hours long and includes exams determining field of vision, mobility, eye movements, postural movement, and balance. He prepares for each appointment by reviewing patient records, medical history, medication, and extent of injury. CNS therapists accompany patients to their appointments, so they may better support this aspect of rehabilitation.
On the first visit, he checks eye health, the optic nerve, retina, macula, and blood vessels. On the second, he works on function, ambulation, gait, balance, and the patient ’s sense of space. To further understand TBI-related impairment, another test is administered which involves an advanced technology called the Visual Evoked Potential (VEP). This is an electro diagnostic test that measures brainwaves associated with the visual pathways. If there is damage along the pathway, the electrical signal in the occipital lobe may be adversely affected.
Creating New Pathways in the Brain
“Along with the different therapies provided at CNS, these procedures and techniques can create new pathways in the brain,” Dr. Garbus said. Progress evaluations help him and CNS clinicians measure improvement and revise therapies. “These evaluations involve more than a typical eye exam,” Dr. Garbus noted. “We have to adjust for speed of processing, dizziness, light sensitivity, and fatigue to identify and treat vision deficits.”
Understanding stroke and TBI are crucial in prescribing glasses specially designed for TBI patients. This usually involves lenses that address specific vision problems, or it may require “prism” glasses to correct visual spatial orientation and eye teaming deficits.
Vision’s Role in Returning to Work
Most patients want to work again, which is a core component of the CNS goal-oriented philosophy. In his years of working with TBI patients, these detailed strategies are worth the effort, Dr. Garbus noted. Many CNS patients return to functionality in real-world settings. “CNS is so good about working at a patient ’s own level of capacity, getting them retrained, inspiring them to volunteer, and helping them to gain a sense of self-worth,” he said.
By William V. Padula, OD and Stephanie Argyris, OD
A person who has suffered a traumatic brain injury (TBI) or cerebral vascular accident (CVA) may often experience difficulties with balance, spatial orientation, coordination, cognitive function, and speech. In most cases, a referral for visual consultation only occurs if there's an injury to an eye or if ocular pathology is suspected. Persons with a TBI or CVA frequently will experience symptoms of double vision, movement of print or stationary objects such as walls and floor, eye strain, visual fatigue, headaches and problems with balance, to name several. Frequently, people will report problems with their vision to rehabilitation professionals and be referred for eye examination. Unfortunately, many will be told that there is nothing wrong with their eye and that it is the effects of their TBI or CVA. Others will be told that their symptoms are not related to their vision.
Visual problems are among the most common sequella following a TBI or CVA, but frequently not dealt with in a rehabilitation model. In order to address visual problems, the Neuro-Optometric Rehabilitation Association is a multi disciplinary institution that provides literature and educational programs for its members. It also serves as a referral source for doctors and rehabilitation professionals who have specific understanding of visual difficulties that arise following a neurological event. A definition of neuro-optometric rehabilitation is: an individualized treatment regimen for patients with visual deficits as a direct result to physical disabilities, traumatic brain injuries, and other neurological insults. Neuro-optometric therapy is a process of rehabilitation to visual/perceptual/motor disorders. It includes, but is not limited to, acquired strabismus, diplopia, binocular dysfunction, convergence and /or accommodation paresis/paralysis, oculomotor dysfunction, visual-spatial dysfunction, visual-perceptual and cognitive deficits, and traumatic, visual acuity loss.
Patients of all ages who have experienced neurological insults require neuro-optometric rehabilitation. Visual problems caused by traumatic brain injury, cerebrovascular accident, cerebral palsy, multiple sclerosis, etc., may interfere with performance causing the person to be identified as learning disabled or as having attention deficit disorder. These visual dysfunctions can manifest themselves as psychological sequella such as anxiety and panic disorders as well as spatial dysfunctions affecting balance and posture.
A neuro-optometric rehabilitation treatment plan improves specific, acquired vision dysfunctions determined by standardized diagnostic criteria. Treatment regimens encompass medically necessary noncompensatory lenses and prisms with and without occlusion and other appropriate medical rehabilitation strategies.
Vision: The Process
The visual system is composed of two separate processes. The process that we are most familiar with has been called the focal process. (Trevarthen2, Leibowitz and Post3). This process is neurologically is related to the central visual function. The eye represents central vision primarily through an area called the macula located in the retina. Aiming your eye directly at an object causes focalization by the brain through the macula.
As noted by Leibowitz and Post, the focal process does not have to be delivered directly by the macula. For example, you can aim your eye at a particular object such as a doorknob on a door across the room. Fixating on the doorknob represents a central focalization. However, you can also focalize with your peripheral vision. While you are aiming your eye at the doorknob, you can use your peripheral vision to focalize on objects about the room, such as a picture or a chair. The focalization process, however is most easily delivered through the macula. While you can focalize in any portion of the visual field, the peripheral vision is primarily used as a general spatial orientation system. The reason for this is that peripheral vision is mostly a function of a second visual process called the ambient process.
The ambient process lets you know where you are in space and provides general information needed for balance, movement, coordination, and posture. Neurologically, nerve fibers from the peripheral retina that are part of the ambient visual process provide axons that are delivered to a level of midbrain where they become part of the sensory-motor feedback loop. The importance of this system is that it is a less sensorially involved and more motoric in function. It must match information with kinesthetic, proprioceptive, vestibular, and even tactile systems for the purpose of orienting and acting as a master organizer of these other processes. Once this is accomplished, a feed-forward mechanism enables this information to be directed to higher cortical areas, including the occipital cortex, as well as 99% of the cortex.
The ambient visual process must let you know where you are in space and essentially where you are looking before you process information about what you are looking at.
Given a neurological event such as a traumatic brain injury (this includes a mild whiplash), multiple sclerosis, cerebrovascular accident, etc., the ambient visual process can lose its ability to match information with other components of the sensory-motor feedback loop. Even a whiplash, as mentioned, can cause significant dysfunction at the level of midbrain. Thomas4 has calculated that at the level of the foramen magnum, as much as 14,000 lbs. of inertial force is exerted on the spinal cord with a minimal 10 mile an hour rear-end collision. This can cause a dysfunction in the sensory-motor feedback loop and more specifically in the ambient visual process. Although this type of an injury cannot be seen in most cases on a CT scan or MRI, injured individuals will frequently experience the types of symptoms explained in the introduction of this paper.
Clinical findings have led the authors to document a new syndrome called Post Trauma Vision Syndrome (PTVS). This syndrome is caused by a dysfunction of the ambient visual process and has the characteristics, as well as symptoms, presented below.
Persons who are not treated for PTVS can experience this syndrome for many years following a neurological event. Treatment of this syndrome may include binasal occlusion in conjunction with low amounts of base-in prism and other types of neuro-optometric rehabilitative approaches, including vision therapy. It has been the author's experience that most cases of PTVS can be treated effectively through neuro-optometric rehabilitation. The authors have found that clinically approximately 15% of persons with PTVS may require more extensive vision therapy.
The significance of this discussion is to recognize that the exotropia, exophoria, accommodative insufficiency, convergence insufficiency, and oculomotor dysfunction are part of the greater dysfunction of the ambient visual process and are essentially characteristics of this function. For example, frequently persons with a diagnosed exotropia after a traumatic brain injury are diagnosed with a 3rd nerve palsy. It has been the author's experience that treating the ambient vision dysfunction through neuro-optometric rehabilitation can in many cases reduce the exotropia. Therefore, the authors question the diagnosis of a neurological/muscular problem without consideration being given to the overall dysfunction of the ambient system causing PTVS when no specific lesion is found by a MRI or CAT scan.
Research has been conducted by the authors utilizing Visual Evoked Potentials (VEP) to capture this state of dysfunction at the level of midbrain5. Subjects were given binocular visual evoked cross-pattern reversal P-100 evaluation with their best distance correction. An experimental group was used in this study. Immediately following phase one of the VEP testing, binasal occlusion and base-in prisms were introduced before both eyes. In the experimental group there was an increase in the amplitude of the VEP.
The increase in amplitude of the binocular VEP for the experimental group when using base-in prisms and bi-nasal occluders suggests that by affecting the ambient visual process through structure from the bi-nasal occluders and field expansion from the base-in prisms, the binocular cortical cells increase in effectiveness. This increase in binocular cortical function is also correlated with the verbal responses from the subjects. Frequently, the subjects reported that the perceived movement of the letters on the chart stabilized. They also reported that it was easier to fixate with two eyes and, for some, the diplopia was eliminated.
This study further indicates that the ocular conditions diagnosed after a TBI may be due to a dysfunction of the ambient visual process in its inability to organize spatial information with other sensory-motor systems. This in turn causes a compromise of the focal process.
This disturbance in the ambient system appears to cause the dysfunction of binocularity for the persons in this study and, for many affected persons, may actually lead to strabismus, convergence insufficiency, accommodative insufficiency and oculomotor dysfunction. It is suggested that, following a TBI, ambient processing dysfunction may be the cause of Post Trauma Vision Syndrome. Understood in this way, the specific binocular dysfunctions are actually characteristic of PTVS.
For more information please contact NORA at noravisionrehab.org
By William V. Padula, OD and Stephanie Argyris, OD
Visual Midline Shift Syndrome
An unusual phenomenon that often occurs following a neurological event, such as hemiparesis or hemiplegia, is that the ambient visual process changes its orientation and concept of midline (the ambient visual process lets you know where you are in space, and provides general information needed for balance, movement, coordination, and posture). To understand this more completely, let us think for a moment about the toddler who begins to gain orientation to a standing posture. The toddler must have organized, at various developmental levels, concepts of visual midline that were established through vestibular, kinesthetic, proprioceptive, and ambient visual processing. These midlines include, but are not limited to, a lateral midline, and a transverse midline. The toddler must gain orientation to the midline in order to develop weight transfer and position sense.
Information from the two sides of the body must be matched through kinesthetic and proprioceptive systems with ambient and vestibular information. This information develops experience and creates a set by which the child continues to process information throughout the developmental years. Given a neurological event such as a CVA causing hemiparesis or hemiplegia, information from one side of the body becomes interfered with. The ambient visual process is a relative processing system. It attempts to create a relative balance based on the information established. With interference of information from one side of the body compared to the other, the ambient visual process attempts to create balance by expanding its concept of space on one side of the body compared to the other. In so doing, a perceived amplification of space occurs internally on one side and a perceived compression of space occurs on the other side. This phenomenon causes a shift in the person's concept of midline, which usually shifts away from the neurologically affected side.
The authors have developed a simple test whereby a wand is passed before the person laterally and the person is asked to state when the wand appears to be directly in front of his nose. A high correlation has been found with a shift in midline away from the neurologically affected side. In other words, the person would frequently report that the object appears to be directly in front of his nose when in fact it may be to the right. This individual will frequently have left-side hemiparesis or hemiplegia. This shift in concept of midline can also occur in an anterior posterior axis, causing the individual to experience a midline shift anteriorly or posteriorly. The result is that posture will be affected by either emphasizing flexion, as in the former, or extension in the case of the latter. Combinations of anterior, posterior, and lateral shift are quite common. While these individuals do have a neurological problem such as a paresis to one side, it has been the author's experience that frequently persons involved in physical therapy will not be able to increase weight bearing on their affected side and/or stand erect without constant reminders from the physical therapist. The therapist will frequently tell the person to stand straight and the person will follow these directions. However, after the physical rehabilitation therapy session is over a shift away from the neurologically affected side continually occurs, frequently causing the person to experience a plateau and therapy to be discontinued.
The authors are stating that there is a visual relationship that occurs through the ambient visual process. However, it must be understood that there are many individuals who do benefit from physical therapy programs and can improve function of their paretic side. Perhaps this is not simply through a strengthening of muscles but really a total change in neurological processing that occurs at the midbrain level in relationship to organization of internal space thereby affecting even the ambient visual process.
Persons with a VMSS will walk as if the plane of the floor is tilted. In fact a number of individuals with VMSS have reported to the authors that the floor appears to be tilted. A neuro-optometric treatment approach that works effectively is to utilize prisms before both eyes positioned in yoked fashion. A prism is a wedge of glass or plastic. The thick end is called the base. When the base ends of the prism are positioned in the same direction for each eye; for example to the right or to the left for both eyes, this is termed yoked prisms. The effect of the prism is to counter the expansion and compression of space that is occurring in the ambient visual process. In turn, this causes the midline to shift to a more centered position.
The authors have noted that clinically persons will frequently shift their weight almost immediately and increase weight bearing on the affected side. The use of these yoked prisms is for short durations each day. The reason for this is that prisms provide a profound change in the ambient visual process and develop a level of experience of weight bearing in relationship to the ambient system as part of the sensory-motor system. The effect will be maintained for longer periods of time throughout the course of rehabilitation. Frequently, the yoked prisms are prescribed to be used in conjunction with physical and/or certain approaches of occupational therapy. These yoked prisms are prescribed following a neuro-optometric evaluation.
Visual Field Loss Affecting VMSS
Visual field loss following a CVA or TBI can often influence a shift in visual midline causing a VMSS. A homonymous hemianopsia frequently occurs following a CVA. The bilateral field loss causes the visual concept of the midline to become centered in the remaining portion of the visual field. In turn, weight bearing will be shifted away from the side of the homonymous hemianopsia producing the effect of the VMSS. Yoked prisms are effective in re-centering the concept of the visual midline and thereby increasing weight bearing on the affected side. Eventually, expanded field prisms can be mounted into the lenses that increase the visual awareness into the side affected by the homonomous hemianopsia.
Conclusion
Persons who have suffered a neurological event have often had visual problems that have been misinterpreted as well as misdiagnosed. Recent advances in research enabling clinicians to gain a better understanding of vision as a process have uncovered more than one visual processing system. The ambient visual process is essentially a silent process. We cannot think in this process. Instead we somehow develop a level of feeling through this process that establishes one's organization of space for balance, movement, and coordination, while also providing a spatial net by which the higher focal process delivers information about detail and identification.
Following a TBI, CVA, or other neurological event frequently individuals lose this ambient visual process and instead are left with a focal processing system that breaks up the visual world into isolated parts. This causes individuals extreme difficulty, not only with balance and movement, but also affects the person in other ways such as in the person's tendency to compress and limit their spatial world. This creates experiences such as an inability to find an object on a shelf in a store. The compression of space causes a focalization process to function both centrally as well as peripherally. This has greater meaning when one thinks of what the experience must be like when all the bottles, cans, and boxes on the shelf is suddenly experienced as massive amounts of detail causing the person to be unable to isolate one detail from another.
Movement in a crowded environment also becomes quite disturbing because the ambient visual process is supposed to assist in stabilizing the image of the peripheral retina. Without this system the person internalizes the movement that he or she is experiencing in the peripheral vision. This become extremely disturbing and causes vertigo, and severe dysfunction. The authors have found that a combination of low amount of base-in prisms and binasal occlusion have been extremely effective in almost immediately offering increased stability to the ambient visual process, thereby reducing the symptoms and enabling the person to re-establish levels of independence that were otherwise not achieved.
Interference caused by Post Trauma Vision Syndrome can also affect higher cognitive functioning. The focal process is very much related to higher perceptual and cognitive function. However, the focal process cannot function properly unless it is grounded by the ambient visual system. In turn, this loss of grounding following PTVS will cause a slowing of responses in general, and interference with higher perceptual cognitive function. Therefore, cognitive therapy should be supported by neuro-optometric rehabilitation.
Neurological problems affecting states of motor function may be diagnosed and even related to specific cortical lesions. However, the total impact of function and performance concerning balance, posture, and movement may be interfered with further by shifts in concepts of the visual midline. The midline with VMSS affects not only persons who are attempting to ambulate, but also those individuals who are wheelchair bound, causing them to lean to the side, forward, or backward. Yoked prism therapeutic lenses can make significant changes in concept of midline, thereby affecting posture, balance, and movement. The use of these yoked prisms can be developed in a transdisciplinary approach, so that they may be incorporated into existing physical and/or occupational therapy programs. The authors again emphasize that neuro-optometric rehabilitation should support the overall rehabilitation of the individual prior to and/or concurrent with physical and/or occupational therapy.
The authors emphasize that these type of neuro-optometric approaches are rehabilitative in nature and should not be thought of as a cure. As with all rehabilitation, progress depends on many factors.
The profound affects of dysfunction in the ambient visual system can greatly interfere with function and performance at all levels for persons with neurological insults. Neuro-optometric rehabilitation has effectively delivered new approaches toward treatment regiments in conjunction with treatment already being conducted in hospitals and clinics. The optometrist who has developed an understanding of neuro-optometric rehabilitation can be an important member of the multi-disciplinary team who is serving these special populations.
For more information please contact NORA at noravisionrehab.org
By John A. Thomas, M.S., O.D.
Post-Trauma vision syndrome (PTVS) describes a constellation of symptoms that evolves as secondary injury in traumatic brain injury. This syndrome includes binocular coordination dysfunctions, disorientation, loss of equilibrium, memory problems, cognitive dysfunction, loss of executive function (including reading), an inability to follow sequential instructions, fatigue, irritability, and sensitivity to light to name the most frequent symptoms. Electrophysiological research suggests that these symptoms are the result of a breakdown in the cellular systems that form the basis of our ambient-focal visual systems (the ambient visual system lets you know where you are in space, and provides the information needed for balance, movement, coordination, and posture. The focal system identifies what you are seeing around you. If the ambient system breaks down, it, in turn, destabilizes the focal system and you cannot maintain a focus on, and properly identify, what you are seeing).
Studies involving brain trauma on animals identifies the molecular basis of neuro disruption resulting in delayed and progressive secondary injury. The molecular mechanism is a breakdown of the intimate association between cerebral blood flow (CBF) and cerebral glucose metabolism (CMGL) causing ischemia (a deficient blood supply) and hypoxia (deficient oxygen supply), which results in metabolic imbalances that change neuronal cell membrane (neurolemma) permeability. Changes in cell membrane permeability immediately result in a cascade of cellular changes that lead to cell toxicity. It is this degenerative neuro-biochemical cascade that results in a delayed and progressive loss of injured-neuron function and is classified as secondary injury. The degree of secondary injury and the rate and extent of progress varies with each individual.
The Visual Operating System
Vision is universally recognized among bioscientists as the dominant ranking sensory perceptual construct of man. Efficient binocular visual perception is the Holy Grail of information processing for Homo Sapiens. Vision is the operating system of the brain. Analogy: Vision is to the brain (visual information processing) as DOS is to the computer, the operating system. Any disturbance in precision visual sensory motor integration or sensory ambient-focal integration results in decompensation and a breakdown of the visual processing systems, resulting in multiple dysfunctions.
It is essential to recognize that cerebral trauma comes in all degrees. No two victims of injury have the same tolerance to the physical forces imposed on the incredibly complex and sensitive central nervous system structure. Like other biological functions, traumatic brain injury comes in all degrees. Existing clinical rating systems, such as the Glasgow Coma Scale, the Ranchos Amigos Scale, presence or absence of consciousness, or velocity statements in police accident reports cannot relate, predict, or correlate the degree of resulting post-trauma vision syndrome. The extent of all secondary injury is not only related to the degree of trauma but is complexly related to victim robustness.
The mild closed head trauma patient is the most frequently under-diagnosed category of traumatic brain injury with secondary injury. Generally, the diagnostic community relies upon loss of consciousness, length of coma, radiological imaging and on occasion neuro-psychological evaluation in the assessment of traumatic brain injury. The noncomatose patient with a negative CT or MRI scan is the classical case. Their symptoms are frequently dismissed as both exaggerated and psychosomatic in origin. This is often disastrous for a mild closed head injury patient and often results in denial of appropriate and necessary rehabilitative services and contributes to the army of walking wounded who look and seem normal but live with generalized cognitive dysfunction.
Clinical Presentation
Drs. William Padula and Stephanie Argyris, in Parts I and II of the Post-Trauma Vision Syndrome series aptly described the primary symptoms of post-trauma vision syndrome to include visual midline shift syndrome (VMLSS). To their list I would add such eye alignment malfunctions as increased esophoria (a tendency to cross eyes) and esotropia (permanently crossed eyes), hyperphoria/hypertropia (one eye up and one eye down), cyclophoria/cyclotropia (rotational misalignment), suppression, photophobia (sensitivity to light), headache, memory deficits, comprehension dysfunction, cognitive dysfunction, compromised reading and writing ability, and the inability to follow sequential instructions. The last seven deficits are classified as executive function disorder. Initial history of the patient, at the scene of the accident and in the emergency room, frequently will not include any comments regarding vision or information processing disturbances. In the absence of obvious facial or eye trauma, or reports of immediate diplopia (double vision), later evolving visual dysfunction symptoms are most frequently dismissed as exaggerated or the result of psychosomatic conversion. This is the result of a lack of appreciation of progressive secondary injury, neuro-biochemical in origin and below the sensitivity of radiological imaging.
The Mechanism
The traumatic forces imposed upon the central nervous system, whether by blunt trauma or whiplash trauma (hyperextension/hyperflexion), cause massive nerve conduction disruptions due to electrical charge changes in cells (depolarization). A breakdown of the connection between CBF and CMGL and membrane permeability changes cause potassium ion losses and an influx of calcium ions. The result is an activation of cellular protease enzymes, which triggers cellular skeletal disruption and simultaneous, excessive neurotransmitter activity. All these factors combine to create an abnormal neuro-biochemical milieu that is degenerative, progressive, and contributes to the degenerative process that erodes the memory imprints controlling the precision of binocular coordination, ambient-focal functioning, and efficient integrated information processing. Thus, the learned and life-long established memory imprints that provided the automatic controls of the very complex sensory motor components of the visual process become eroded. The result is degradation of our dominant sensory perception, our dominant guidance system: visual information.
Management
Aggressive neuro-biological and pharmacological research yields agents that can control excess neurotransmitter activity by blocking certain receptor sites, blocking production of endogenous opioids (such as endorphins), blocking enzymatic activity, causing selective enzymatic activity, stabilizing cell membranes, and neutralizing free radicals, thus providing a degree of control over progressive secondary injury. However, controlled studies of these substances and their utilization have been restricted to animals. No approved pharmacological interventions exist for human use.
Discussion
Multiple advanced technologies have confirmed that the cell-toxic neuro-biochemical milieu that results in cell structure collapse and progressive secondary injury, also results in decreased cerebral competence such as: post-trauma vision syndrome, compromised executive function (including cognitive skills loss), reading dysfunction, and general degradation of cognitive function. Extensive research has provided a sound neuro-biochemical basis to include the elements of post-trauma vision syndrome in explaining the previously unexplainable symptoms, with late onset and progression, of secondary injury.
Conclusions
Neuro-biologists are working aggressively to establish pharmacological interventions to minimize the progressive neurological insult described above. Present pharmacological intervention is primarily relegated to severe traumatic brain injury and includes a handful of old standbys, which include naloxone, dextromethorphan, methylprednisone, furosemide, and the antioxidant family. Only the family of antioxidants is clinically applicable to a mild closed head injury case.
As described in the previous segments of this series, neuro-optometric rehabilitative treatment has been enormously successful in contributing to the reordering of the visual information processing coordinant systems essential to reestablishing the visual guidance faculty. I confirm Drs. Argyris? and Padula?s statement that neuro-optometric rehabilitation needs to be concurrent with, or preceding, other rehabilitative strategies. This is essential and prerequisite to any cognitive rehabilitative therapy. Attempts to provide cognitive rehabilitation in the presence of post-trauma vision syndrome is equivalent to throwing back the ocean with a bottomless bucket. Without an intact, coordinated, and integrated binocular vision processing faculty, cognitive rehabilitation is futile, frustrating, and frequently results in a premature pronouncement of maximum medical achievement. Neuro-optometric rehabilitation is an essential component of the transdisciplinary rehabilitative team essential to the restoration of integrated function.
For more information please contact NORA at noravisionrehab.org
The Visual System involves complex actions and interactions of the eyes and the brain. To simplify this description, the Visual System is being placed into three areas of function: acuity, perception, and eye movement. Any one of these functions can be impaired without impairment to the remaining two functions. Or, all functions may be impaired as the result of MTBI. The extent of injury will depend upon the force to and location of trauma in the brain. Dysfunction in any of these areas may contribute to headaches, fatigue, and/or dizziness.
Acuity or How Sharply You See
The Eye and the Optic Nerve
As light enters the eye it travels through the cornea, lens and retina (the neural part of the eye). At this point, the image of what is being seen is processed, reversed and transmitted along the optic tracts (visual pathways). The image is carried via the optic tracts through the brain to the Occipital Lobe (primary visual cortex) at the back of the brain.
The eye can be injured by a direct blow which may injure the cornea, lens, retina, and/or optic tract. Blurred vision or partial visual loss can result from this injury which may be transient or improve with treatment or may be permanent.
Perception or Interpreting What You See
The Occipital Lobe
This lobe sits at the back of the brain and receives the images transmitted to it from the optic tracts. A blow to the occipital lobe (back of the head) may result in an inability to make sense of what you see (visual agnosia) in your environment or read in a book or newspaper. The worst result would be "cortical blindness", an inability to see anything secondary to impaired interpretation of what is seen. This condition may be permanent or transient.
Control of Eye Movements
The superior colliculus and paramedian pontine reticular formation (brainstem)
Each eye has approximately six muscles. Each muscle independently controls an eye movement. Each muscle is individually controlled by one of three Cranial Nerves: III, IV, and VI. Normal eye movements are synchronized to present reflections onto the retina to result in a single image. If any one or all of the three Cranial Nerves are damaged the eye movement and synchronization are altered and two images may be seen. This is double vision or diplopia. Double vision may exist in all fields of vision or only in certain areas.
Independently activated eye movements involve different areas of the brain:
Saccades, movement on command, and searching movement (pons - brainstem)
Slow pursuit or tracking a moving object (occipital lobe)
Vestibuloocular reflex eye movement (VOR): keeps the eye fixed on an object while the head in moving. (brainstem and vestibular system)
Vergence eye movements: influence by areas in the occipital lobe to keep both eyes on an object whether near or far
Other vision problems related to MTBI
CNS Monthly Newsletter
The latest CNS updates, including events, company information, and patient care developments
The Inside View
Quarterly magazine focused on brain injury research, rehabilitation, and advancements shaping the field
Sign-up for one or both to stay connected with brain injury news and recover


